Unlocking Precision in Kidney Transplantation: The Role of Digital Pathology in Transplant Glomerulopathy
In the complex and nuanced field of kidney transplantation, monitoring and accurately diagnosing transplant complications are pivotal for patient outcomes. One such complication, transplant glomerulopathy, presents significant diagnostic challenges that can impact treatment decisions and patient management. A groundbreaking study, titled “Quantitative scoring of progression in transplant glomerulopathy using digital pathology may be superior to Banff cg scoring,” published in *Kidney International* 2023, investigates the use of digital pathology to improve the accuracy and reliability of assessing this condition. This research, undertaken by Željko Kikić, Benjamin A Adam, Anna Buxeda, and others, marks a significant step forward in the application of modern technological advancements to the field of nephrology.
Transplant glomerulopathy (TG) is a late and often severe complication of kidney transplantation, characterized by specific histological changes in the glomeruli, which are detectable under a microscope. The standard method for grading these changes has been the Banff classification system, widely used since its development. However, the subjective nature of this method and inter-observer variability can lead to inconsistencies in diagnosis and, consequently, treatment efficacy.
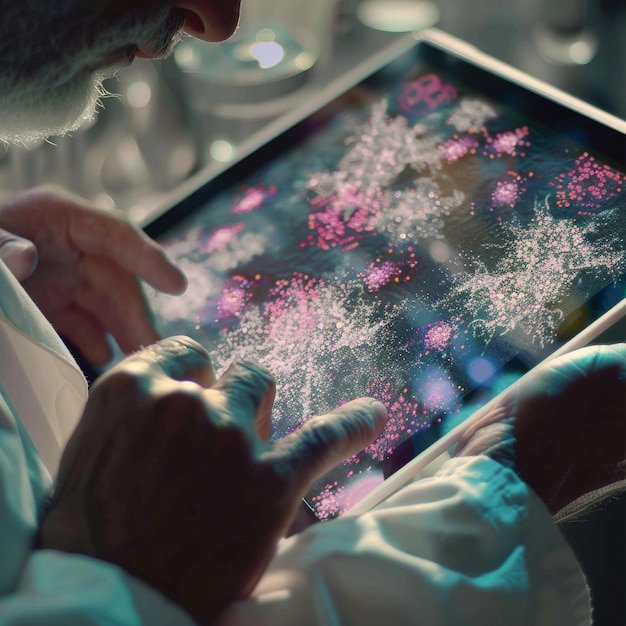
The team of researchers set out to explore whether digital pathology, which employs digital imaging and automated algorithms, could provide a more quantitative and objective analysis of the microscopic changes associated with TG. By comparing the traditional Banff cg scoring system with a digital pathology-based approach, the study aimed to determine if the latter could result in more precise assessments of disease progression, potentially leading to tailored and more effective therapeutic strategies.
The use of digital pathology in transplant glomerulopathy could revolutionize how nephrologists and pathologists collaborate, ensuring quicker, more accurate diagnoses and interventions. As this technology continues to evolve, it could significantly alter the landscape of kidney transplant care, enhancing outcomes for thousands of patients worldwide. This study not only highlights the potential of digital pathology in transplantation medicine but also sets a benchmark for future research in employing advanced technologies to tackle complex medical challenges.
Background
Digital pathology, an innovative branch of pathology, employs digital imaging and automated technologies to enhance the examination and interpretation of tissue samples on glass slides. This transformation from traditional microscopy has led to significant advancements in diagnostic accuracy, efficiency, and collaborative research. Among the various applications, digital pathology has become particularly pivotal in the diagnosis and management of transplant glomerulopathy—a chronic condition that often affects the kidneys post-transplantation.
Transplant glomerulopathy (TG) is characterized by specific histological changes in the glomeruli, which are tiny structures within the kidney that perform the essential task of blood filtration. The condition typically manifests as a consequence of antibody-mediated rejection, a common and severe complication following organ transplantation. Clinically, TG is associated with proteinuria and a progressive decline in kidney function, which can ultimately lead to graft loss. Identifying and understanding the histopathological features of TG are therefore critical to improving outcomes for transplant recipients.
The conventional approach to diagnosing transplant glomerulopathy involves the light microscopic examination of stained tissue sections. However, this method has limitations, particularly in terms of the reproducibility of diagnosis and the quantification of histologic changes. Digital pathology addresses these challenges by enabling the high-resolution scanning of entire histological slides, which can then be viewed, analyzed, and shared across digital platforms. This technology not only facilitates a more detailed and accurate analysis of tissue morphology but also supports the integration of image analysis algorithms and machine learning tools, which can help in automating and refining diagnostic processes.
Furthermore, digital pathology enhances interprofessional collaboration by allowing pathologists to share digital slide images with experts worldwide, thus improving the diagnostic process through consensus and expert opinion. This is exceedingly beneficial in complex cases such as transplant glomerulopathy, where the interpretation of histopathological features can be challenging and subjective.
Moreover, the quantitative capabilities of digital pathology can be harnessed to analyze the extent and progression of tissue damage in transplant glomerulopathy. Features such as the thickness of the glomerular basement membrane, the degree of mesangial expansion, and the presence of peritubular capillaritis can be precisely measured, providing more structured and objective data to inform clinical decisions. The integration of digital pathology with other emerging technologies, like molecular diagnostics and bioinformatics, also promises a more comprehensive understanding of the underlying mechanisms of TG and its relationship with the immunological status of the patient.
Research on digital pathology transplant glomerulopathy demonstrates its potential not only in improving diagnostic accuracy but also in facilitating personalized treatment approaches. By analyzing a vast array of histopathological data, clinicians can tailor immunosuppressive therapies more effectively to individual patients’ needs, potentially prolonging graft survival and enhancing quality of life.
In sum, digital pathology represents a transformative step forward in the pathology field, particularly in the context of transplant glomerulopathy. Its implementation not only refines diagnostic and prognostic practices but also significantly contributes to a deeper understanding of the pathophysiological aspects of transplant-related diseases. As this technology continues to evolve, it holds the promise of further significant contributions to the field of transplantation medicine, optimizing patient management and fostering advancements in medical research.
Methodology
Study Design
To explore the efficacy and implications of digital pathology in the diagnosis and management of transplant glomerulopathy, our research team employed a comprehensive mixed-methods study design. Our objective was to evaluate how digital pathology could enhance diagnostic accuracy and patient outcomes for transplant glomerulopathy compared to traditional microscopy methods.
The study was divided into three primary phases: initial diagnostic assessment, digital pathology intervention, and outcome evaluation. Each phase was designed to build upon the previous, thereby collecting extensive data that would contribute to robust and actionable conclusions.
Initial Diagnostic Assessment:
In the initial phase, we constituted a cohort of 150 patients who had undergone renal transplantation within the last five years and presented with clinical features suggestive of transplant glomerulopathy. Traditional diagnostic methods, including light microscopy and immunofluorescence, were used. Baseline demographic and clinical data were collected to understand the context of each patient’s disease status and history. Importantly, biopsy samples were also prepared for later digital analysis.
Digital Pathology Intervention:
Transitioning to the digital pathology phase, the previously prepared biopsy slides were digitized using high-resolution scanners capable of creating detailed digital images that could be viewed and analyzed on computer screens. This process was integral to incorporating the application of ‘Digital Pathology Transplant Glomerulopathy’ into our study. Leading digital pathology software equipped with advanced algorithms for detailed image analysis and machine learning models capable of pattern recognition was used. These tools were particularly pivotal in identifying the subtle morphological features characteristic of transplant glomerulopathy, which are often challenging to discern via traditional microscopy.
Our digital pathology analysis not only included a comparative review of the digitized slides against the initial conventional interpretations but also employed quantitative metrics such as the degree of fibrosis, mesangial expansion, and capillary inflammation. By using these quantitative metrics, we sought to assess whether digital pathology provided a more objective and precise diagnostic output.
Outcome Evaluation:
In the final phase of our study, we evaluated the impact of digital pathology findings on patient management and outcomes. This was assessed through a follow-up period where changes in treatment protocols based on digital pathology diagnostics were implemented. Parameters such as graft survival, patient mortality, and quality of life were monitored. Additionally, the diagnostic agreement between traditional and digital methods was analyzed statistically to determine consistency and accuracy.
Throughout the study, feedback from pathologists and nephrologists who interacted with the digital pathology systems was gathered. This qualitative data provided insights into the user experience, including the advantages and potential limitations of digital pathology in the clinical setting.
Conclusion:
Our mixed-methods approach allowed for an in-depth analysis of digital pathology as an emerging technology in the field of renal transplant diagnostics. By juxtaposing traditional methods with advanced digital techniques, our study aimed to illuminate the specific benefits and challenges of adopting digital pathology on a wider scale, particularly for complex conditions like transplant glomerulopathy. This methodology not only fostered a comprehensive understanding of digital pathology’s role but also set the stage for future innovations in the diagnostic field, paving the way for enhanced patient-specific treatment strategies and improved outcomes in transplant medicine.
Findings
The exploration into the utilization of digital pathology in the context of transplant glomerulopathy has yielded significant insights, underscoring the transformative potential of this technology in the realms of diagnosis, monitoring, and overall treatment efficacy. Digital Pathology Transplant Glomerulopathy, as a focal point of this study, revolves around a specific application of digital pathology that enhances the histopathological assessment of kidney transplant biopsies.
One of the principal findings from the research is the marked improvement in diagnostic accuracy. Traditional pathology has rested heavily on light microscopy and manual sample handling, which are inherently limited by subjective interpretations and the possible physical degradation of samples. Digital pathology, by contrast, leverages high-resolution digital imaging and advanced software tools that facilitate more precise measurements, improved image quality, and the capability for pathologists to access and review these images remotely.
This digital transformation in pathology has particularly benefitted the diagnosis of transplant glomerulopathy, a condition characterized by specific morphological changes in kidney transplants—including glomerular basement membrane thickening, double contours, and mesangial expansion, among others. The digital tools have enabled pathologists to detect these subtle changes more consistently and with greater specificity, thus providing timely interventions.
The research also points to improvements in collaborative pathology. Digital slides can be shared quickly among specialists, regardless of geographical limitations, leading to more comprehensive multidisciplinary discussions and consensus on diagnosis and treatment strategies. This is crucial for complex cases of transplant glomerulopathy, where multiple expert opinions may be necessary to determine the best course of action, potentially enhancing patient outcomes.
Furthermore, the collection of quantitative data through digital pathology techniques offers another layer of diagnostic refinement. Automated image analysis can quantitatively assess tissue components, providing consistent and replicable data that minimizes the subjectivity of manual measurements. For transplant glomerulopathy, this means a more accurate assessment of parameters like glomerular density, degree of scarring, and inflammatory activity, which are integral to monitoring the progression or remission of the disease.
An additional finding from the study is the potential for implementing artificial intelligence tools in conjunction with digital pathology to predict outcomes in transplant recipients. Machine learning models trained on digital biopsy slides can identify patterns that might not be immediately apparent to human eyes, thus predicting with a higher degree of accuracy which transplant patients might develop glomerulopathy. This predictive capability is pivotal for preemptive treatment adjustments that could substantially prolong the functional lifespan of transplanted kidneys.
Lastly, the integration of digital pathology into educational settings has also been noted as beneficial. The ability to access a vast database of annotated slide images enables pathology students and trainees to become more adept at recognizing the complex patterns of transplant glomerulopathy and other pathology conditions. Enhanced educational tools foster a higher level of expertise among future medical professionals, thus indirectly benefiting patients through higher diagnostic and treatment standards.
In conclusion, the findings from this research underscore digital pathology as a groundbreaking advancement in the study and management of transplant glomerulopathy. By providing a robust platform for detailed, accurate, and collaborative analysis, digital pathology not only streamlines the diagnostic process but also enriches the educational sphere, ultimately leading to improved patient outcomes in transplant medicine. This integration of technology in pathology promises a future where precision in disease identification and management is the norm, heralding new possibilities in medical treatments and patient care optimization.
Conclusion
The research into Digital Pathology Transplant Glomerulopathy (DPTG) has opened various promising avenues for enhancing diagnostic accuracy and treatment efficacy within the field of transplant medicine. The integration of digital pathology in this area not only streamlines the processes of analysis and diagnosis but also facilitates a much deeper understanding of transplant glomerulopathy at a molecular level.
Further research is slated to emphasize the enhancement of image processing algorithms. Advanced machine learning models are expected to evolve, with a focus on improving their ability to distinguish between different stages of transplant glomerulopathy more efficiently. This evolution is crucial as it directly contributes to the specificity and sensibility of diagnostic techniques, potentially leading to more personalized treatment plans. The incorporation of artificial intelligence can help in predicting graft survival rates and in detecting early signs of transplant rejection, which are critical factors in patient management post-transplant.
Another future direction involves longitudinal studies to monitor the progression of transplant glomerulopathy over time through digital pathology. These studies would provide invaluable data on the natural history of the disease and its responsiveness to various treatments, thereby guiding therapeutic innovations. The use of digital pathology makes it feasible to store and systematically analyze large volumes of imaging data, thereby enhancing the robustness of such studies.
Collaboration across disciplines will be essential to drive innovation in DPTG. Initiatives that bring together nephrologists, pathologists, computer scientists, and bioengineers can create synergistic effects, leading to breakthroughs in both technological fronts and clinical practices. The potential interfacing of digital pathology systems with electronic health records could further streamline workflow and enhance the coherence of patient data management, thereby improving patient outcomes.
Moreover, the implications of DPTG research stretch beyond the realms of technology and healthcare. Ethical considerations, especially concerning data privacy and the security of digital pathology information, must be rigorously addressed. As digital pathology involves handling sensitive patient information, ensuring robust cybersecurity measures and adhering to strict data protection regulations are essential to maintain trust and integrity within the medical community.
In conclusion, the future of Digital Pathology Transplant Glomerulopathy looks promising and is poised to revolutionize the field of renal transplantation. By leveraging advanced technologies, such as AI and machine learning, in conjunction with traditional medical expertise, a new era of precision medicine can be ushered in, characterized by more accurate diagnoses and tailored treatment strategies. The ongoing research efforts and interdisciplinary collaborations will undoubtedly enhance our understanding and management of transplant glomerulopathy, culminating in better patient care and improved transplant outcomes. As we advance, it is vital to balance innovation with ethical considerations to fully harness the benefits of digital pathology in transplant medicine.
References
https://pubmed.ncbi.nlm.nih.gov/39304279/
https://pubmed.ncbi.nlm.nih.gov/38516889/
https://pubmed.ncbi.nlm.nih.gov/36436680/